Visits: 13
Q. Define Horner’s syndrome.
Ans. A lesion in the oculosympathetic pathway resulting in the classic triad of (partial) ptosis (droopy eyelid), miosis (pupil constriction), and variable degrees of anhidrosis (loss of hemifacial sweating) which is usually ipsilateral
Q. Describe the sympathetic innervation of the eye
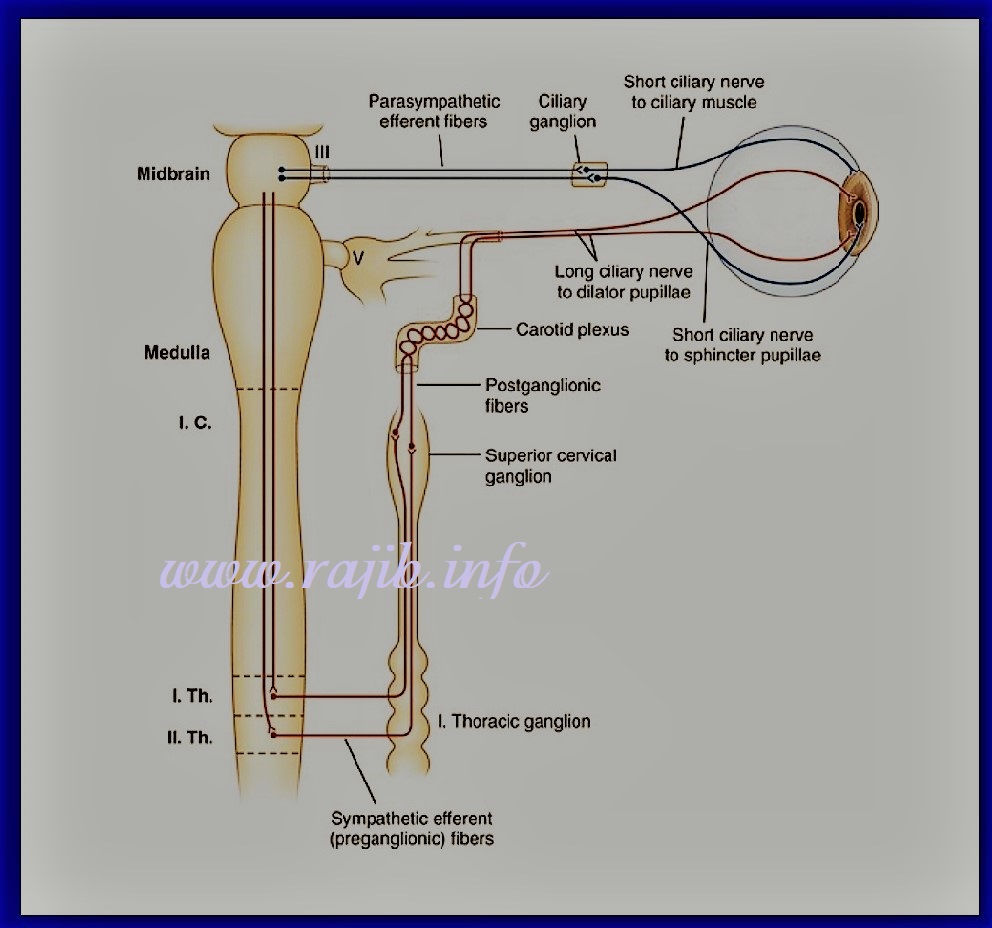
Ans. 3 neuron pathway:
> First-order fibers arise from the hypothalamus, descend and terminate at the level of C8-T1
> Second-order preganglionic pupillomotor fibers exit the spinal cord at the level of T1 and enter the stellate ganglion (sympathetic trunk), where they are in close proximity to the pulmonary apex and the subclavian artery
Then they ascend through the sympathetic chain and synapse in the superior cervical ganglion (SCG) at the level of the bifurcation of the common carotid artery (C3-C4).
> Third order postganglionic fibers give off sudomotor branches to the sweat glands of the face just above SCG
Ascending postganglionic fibers travel through the carotid plexus and eventually join the long ciliary nerves which innervate the dilator pupillae and the superior tarsal muscle (involved in raising the superior eyelid).
Q. Describe how the location of the lesion affects anhidrosis.
Ans. First-order neuron lesions → ipsilateral anhidrosis
Second-order neuron lesions → possible ipsilateral anhidrosis
Third-order lesion → anhidrosis is either absent or limited to an area above the ipsilateral brow (postganglionic lesions occurring after vasomotor and sudomotor fibers have branched off the sympathetic chain)
Q. Describe enopthalmos (posterior displacement of the eye within the orbit) in relation to Horner’s
Ans. Early literature frequently mentions enophthalmos as a sign of Horner’s syndrome, but this is a flawed observation. The apparent enophthalmos is due to the narrowed palpebral fissure, and true enophthalmosis not present with Horner’s syndrome in humans
Q. Describe why miosis occurs in Horner’s.
Ans. Interruption of the oculosympathetic pathway to the pupillary dilator muscle results in a smaller pupil on the affected side, as the parasympathetic tone to the pupillary constrictor muscle is unopposed
Q. What is the classic cause of a second-order neuron lesions?
Ans. Pancoast tumour.
Also caused by metastases, chest surgery, thoracic aortic aneurysms, or trauma to the brachial plexus.
Q. Define Pancoast tumour.
Ans. Criteria: Tumor must invade the parietal pleura and cause pain, paresthesias or other neurological dysfunction; it is not sufficient only to have an apical lung tumor.
Often it’s also called a superior sulcus tumour (SST) due to the anatomical groove present in the lung apex, formed by the subclavian artery as it passes over the lung at this point.
Q. Describe how the anatomical location of a Pancoast tumour affects the pathology.
Ans. These tumors may invade muscles, upper ribs, thoracic vertebral bodies, subclavian vessels, the inferior portion of the brachial plexus, and the stellate ganglion.
Invasion of the stellate ganglion → Horner’s syndrome
Invasion of all 3 mentioned above → Pancoast syndrome.
Q. Define Pancoast syndrome and describe its clinical features.
Ans. A Pancoast tumour causing destructive lesions of the thoracic inlet accompanied by the following:
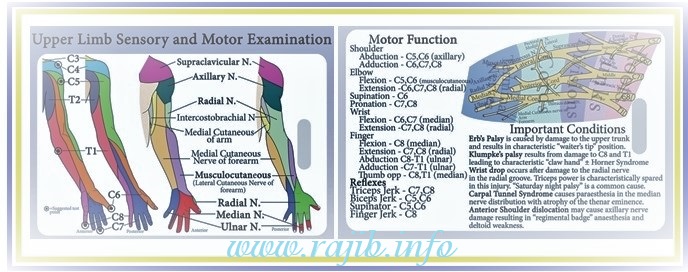
> Shoulder / arm pain region radiating toward the axilla and scapula and along the distribution of the ulnar nerve (C8-T2 nerve roots)
> Atrophy of intrinsic muscles of the hand, particularly the interosseous muscles
> Horner’s syndrome
> Upper limb swelling and discoloration
Q. Describe how a Pancoast tumour can cause upper limb swelling and discoloration.
Ans. As the tumour grows, it partially or completely compresses the subclavian vein
> Oedema and cyanosis results as a failure of venous drainage
> Tenderness, erythema and warmth may present
Q. What symptom is likely to present if a Pancoast tumour affects the C8 nerve root?
Ans. C8 → Pain / loss of sensation in the medial two digits of the hand
Q. What symptom is likely to present if a Pancoast tumour affects the T1 nerve root?
Ans. T1 → pain radiating down / loss of sensation in the medial aspect of the arm as far as the wrist
T1 myotome is in the hand → loss of function; T1 involvement is most common with a Pancoast tumour
Q. A Pancoast tumour is most commonly what type of tumour?
Ans. Most Pancoast tumours are non-small cell lung cancers – squamous cell carcinomas or adenocarcinomas
Q. What diagnostic test can you use for Horner’s?
Ans. Cocaine test: administration of topical cocaine blocks the reuptake of NA at the NMJ. Patients with Horner’s have minimal to no release of NA ∴ cocaine administration will have mininal to no effect on miosis
Q. What diagnostic tests would you use to look for a possible pancoast tumour.
Ans. Imaging: CT/MRI/PET [ > MRI most sensitive and specific; > CXR – not great]
Biopsy – needed for histological confirmation, operability assessment and therapy planning (mandatory prior to definitive treatment); Neurologic examination is essential for assessment of nerve root involvement
Q. Describe treatment for a Pancoast tumour.
Ans. Chemo-radiotherapy with the possibility of complete tumour resection
Less than 50% of patients with Pancoast tumors are considered resectable lesions
(Collected from internet)